I’m afraid nobody will read this article because the headline sucks… I’ve thought about it over and over but ain’t found anything better.
The problem is: inside MASTERING DENTISTRY there’s a sort of in-fighting between Stefano and me. Whoever gets more accesses to his posts wins. Till some weeks ago my record was undisputed but now, after Stefano’s article about Thermafill, he is breathing down my neck.
Even if this article will not help me destroy my partner I have to write it because it’s about a very important topic. Above all for young colleagues starting their surgical practice.
Let’s start from the lie they told me at university: “when you extract an impacted wisdom tooth the patient swells because you have touched the bone… the longer you let the flap open the more the swelling”.
Dogma! Absolutely irrefutable! It has been a while since I last attended university and I don’t know what they’re telling there nowadays but I wouldn’t be surprised if the story was the same.
But then I wonder why Mrs Virginia who I operated last week during a live surgery course:
- Exposing the bone of a great part of the mandible
- Doing a 10mm vertical osteotomy of the knife edged ridge
- Keeping the flap open for about 50 minutes because of the live surgery explanation time
- Doing four 3,5×15 mm diameter holes in the bone
… the day after the surgery looks like that?
This questions the “university dogma” pretty much!
Actually I can’t really tell you what the post-op symptomatology depends on because a lot of RCT should be done comparing all possible factors over a lot of patients. I think that in this field the best option is to rely on the experience of high performing surgeons. I can tell you that a zone where the patient usually swells like a bagpipe is precisely the posterior mandible where the most frequent surgeries are impacted wisdom teeth extraction and bone harvesting from the ramus.
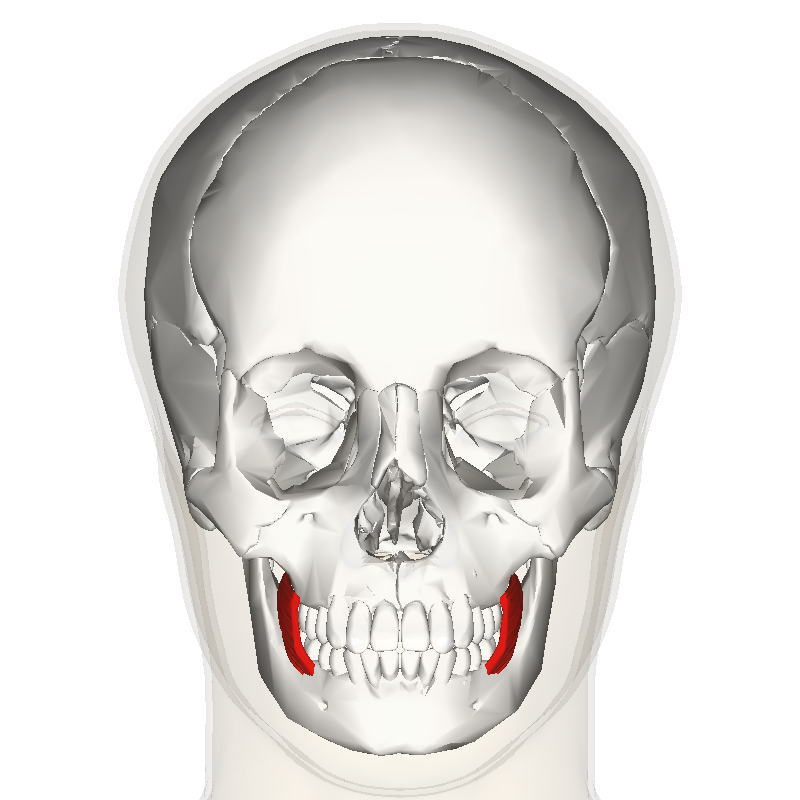
I think I know why that zone is so annoying. Look at this image:
The red stuff is the buccinator muscle. Laterally and a little behind there is the masseter muscle.
Let’s imagine what happens when you plunge the blade buccally to second or third molar to perform a vertical incision: you’ll cut the buccinator muscle and probably also the masseter one if you drop the hammer. That will cause at first a great bleeding that will break your balls all along the procedure, and then a long and “amusing” healing period for your patient.
This is the case if you happen to be lucky. When you (and your patient) are unlucky… take a look below:
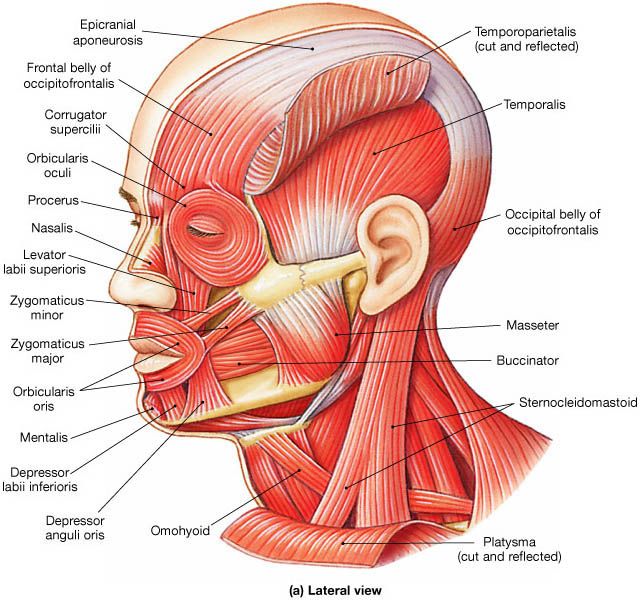
The yellow structure that goes from the lingual side to the buccal side over the mandibular ramus is the buccal nerve. It innervates in a sensitive way the mucous membrane and the skin of the cheek and to get there it pierces the buccinator muscle going through it.
IN CONCLUSION,
if you manage the scalpel as an hammer in the muscle, along with increasing bleeding, pain and swelling, you will be likely to cause a relevant neurological damage to your patient. That’s why the vertical incision in the posterior mandible requires some tricks I’m showing you in the beautiful video below.
Remember that soft tissue management always comes BEFORE and AFTER hard tissue management, that unfortunately is often the only one we focus on.
Our online course that will solve all your doubts about soft tissue management is now available here.
And now let’s watch the video! It stops at some point to give me time to explain but don’t worry it’ll start again.