Here we are talking about boring biology. But don’t lose heart: try to reach the end of the article, down there you’ll find a great 4k surgical video!
Something like a month ago I went to the Italian Accademy of Osteointegration closed meeting and I attended a very interesting talk about bone regeneration.
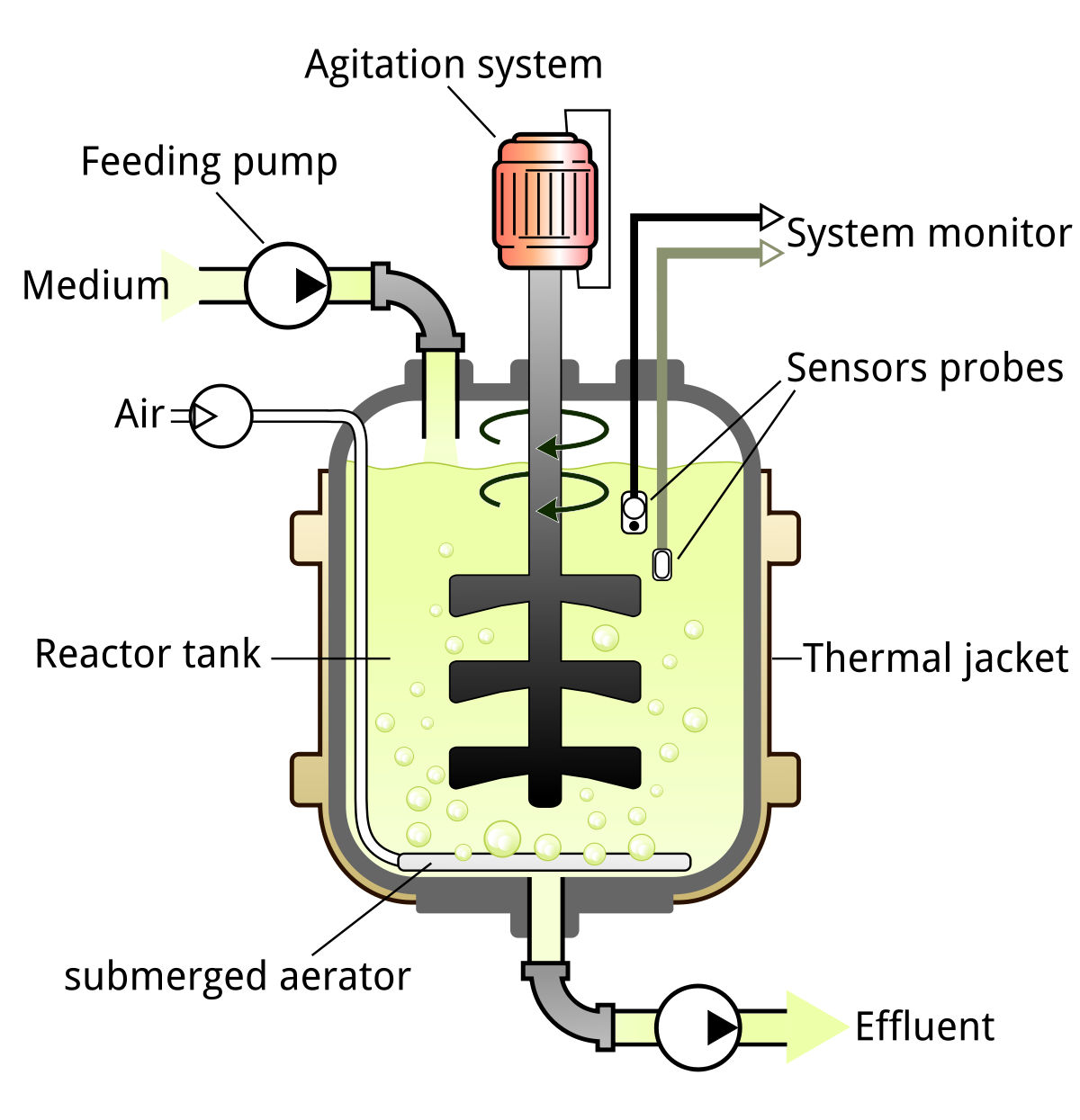
The concept I loved more, that I want to share with you, is the comparison a young biologist made between the grafted site and a BIOREACTOR.
Don’t worry if you don’t know what a bioreactor is. Me neither back then.
More and above all:
“A bioreactor may also refer to a device or system meant to grow cells or tissues”
Oh, boy, that’s exactly what we are supposed to do! We have to get new bone where it ain’t present yet and mostly where it doesn’t wanna grow anymore!
So we just have to build a bioreactor in our patient’s bone defect and we’ll get, as a result, the tissue regeneration we desire so badly.
The bioreactors used in cartilage tissue engineering must have a key feature. They have to provide some kind of mechanical stress to the tissue during its formation. That’s because the cartilage, that is a connective tissue, is formed in parts of the body (like joints) that undergo strong mechanical stresses in order to provide a sort of buffer against the arduous effect of the stresses.
But then, if the mesenchymal cells that arrive in our surgical wound while performing a reconstructive surgery, undergo mechanical stresses and movement they will differentiate in that same direction.
Simply put: if the cells receive some “movement” information their answer will be connective differentiation.
So if the stuff we put in a patient’s defect moves we have built an enviable bioreactor for cartilage tissue engineering. The great trouble is that our titanium implants don’t work so well when put in connective tissue. You know those implants with slight mobility… if you beat them they make a thud… and the patients say “they feel something”?
That’s why it’s better to put some bone around implants!
So, the “oral bioreactor” we have to create must be very different from the ones used for cartilage tissue engineering. As far as possible it has to prevent mesenchymal cells from mechanical stress so that they can (perhaps.. in case we respect the other two secrets) differentiate in bone cells.
AND WHERE DO THE MESENCHYMAL CELLS STAY INSIDE OUR WOUND??
IN THE CLOT.
SO WHAT DO YOU NEED TO OBTAIN BONE REGENERATION?!?!?
CLOT STABILITY
Please let me ask another impressive question…
AND SO WHAT IS THE FUNCTION OF THE MEMBRANE?!?!?! TO PREVENT THE GUM FROM “EATING” THE BIO-OSS?!?!?!
NOOOOO!!!!!
THE MEMBRANE IS ABOUT CLOT STABILIZATION!
And we need it when the clot hasn’t got enough self stability.
This whole reasoning, shows us why a sinus lifting procedure works even if performed by Mikey Mouse putting some cheese inside there. What kind of clot could be more stable but the one that forms on the bottom side of the sinus.
All this argument is aimed at revealing the first secret of bone regeneration in implantology.
1)When you perform some kind of bone regeneration the biomatherials you use are intended for stabilizing the clot that contains mesenchymal cells that will differentiate in bone cells.
So if you use a membrane you have to firmly fix it and stretch it like a forty weeks pregnant woman’s belly, (and I’m speaking about twin pregnancy!)!
But we still have to consider two more bioreactor key factors:
- The presence of biochemical signals that induce cell differentiation. The favourable stabile surrounding is not enough, indeed. And…
- The protection against bacterial and chemical insults that are quite engaging in the human mouth.
These two needs lead us to the second and third secret.
2) Inside your clot something is needed to provide biochemical signals for the bone regeneration to be induced. And from my point of view this something, to this day, is embodied by autologous bone. So the more the greatness of the defect the more the need of autologous bone to be used because some biomaterial particles are very far from residual bone walls.
By mixing particulate autologous bone in the biomaterial you will spread lots of little bone walls in your clot and they themselves will spread useful signals for bone regeneraton.
And last but not least:
3) All this plenty of mechanically stable and osteoinductive stuff has to be protected from external insults, from bacteria and oral fluids, by a great and powerful soft tissue management that can allow you to tight close the wound even if you have increased the bone volume a lot.
If you perform a reconstruction properly but then you are not able to close the soft tissues everything will go tits up, both your efforts and your money.
This is the reason why we’ve decided to design an online course focused only on SOFT TISSUE MANAGEMENT in implant and periodontal surgery. Without theoretical bullshit. Made only by high quality commented surgical videos that will show you all the steps and all the tricks you need for the good management of an aspect that has taken the backseat for long.
SO STAY TUNED.
But let’s start from scratch, I leave you a video about the first secret.